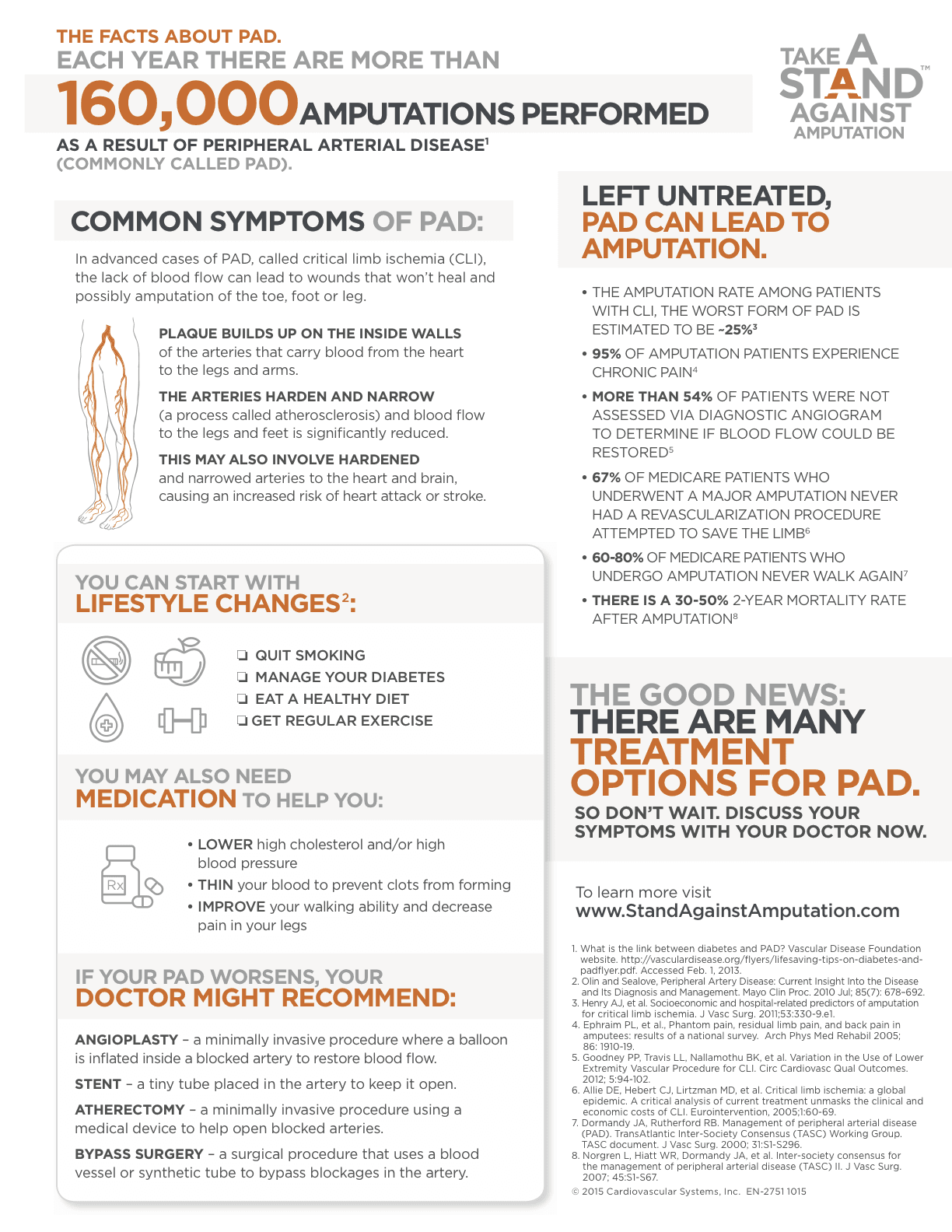
A NY Times Health Care blog published in April of 2016 screamed out with the title “Millions With Leg Pain Have Peripheral Arterial Disease”.”More than eight million older Americans have a condition that can cause leg pain when they walk even short distances. Yet half of those who have the condition don’t know it and consequently don’t get treated for it, putting themselves at risk for a heart attack, stroke or worse.The condition, called peripheral artery disease, or P.A.D., is marked by diseased or blocked arteries in the legs. More than half of those with such circulatory problems in the extremities also have coronary or cerebral artery disease, noted Dr. Iftikhar J. Kullo, a cardiovascular specialist at the Mayo Clinic, in The New England Journal of Medicine in March. Failure to diagnose and treat blocked arteries elsewhere in the body can result in more serious, or even fatal, problems if they affect the heart or brain.It may seem odd that people who have serious difficulty walking normal distances would not know something is wrong and get checked out. Yet, as Dr. Kullo noted, P.A.D. is both underdiagnosed and undertreated. And the number of cases of P.A.D. is only likely to rise as the population ages, he said.”The article in its entirety can be read by clicking on the link below
https://well.blogs.nytimes.com/2016/04/11/millions-with-leg-pain-have-peripheral-artery-disease/
San Jose’s South Bay Vascular Center surgeons specialize in the care and treatment of patients suffering from PAD. Recognized as one of California’s leading Vascular Surgeons, Dr Kokinos has a special interest in peripheral re-vascularization procedures. Essential to her success in treating PAD is her ability to perform these re-vascularization procedures in her nationally accredited, custom built, state of the art peripheral arterial disease (PAD) treatment center. This facility, located in Campbell, CA., was specifically designed as a PAD treatment facility and is where South Bay Vascular Center physicians leverage advanced imaging systems (Ziehm C-Arms with Flat Panel Detectors and Phillips Intra Vascular Ultrasound imaging systems) to provide the most advanced surgical techniques available in this area. This advanced technology, together with a vast inventory of specialized medical devices not found in traditional operating rooms allows our surgeons to perform advanced, minimally invasive surgical procedures in their efforts to provide the best possible outcomes in the most difficult circumstances.Diagnosis
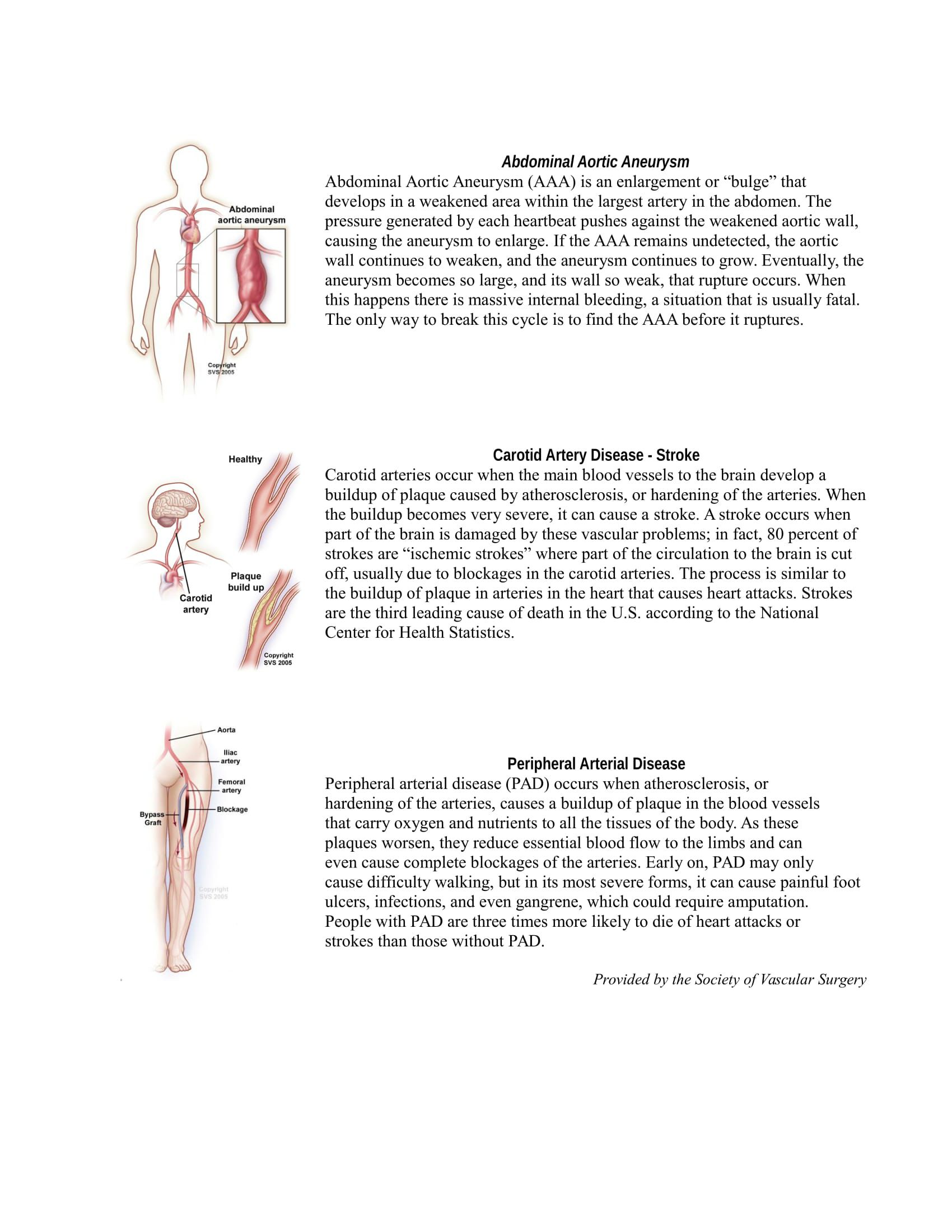
Many types of health care providers can diagnose and treat PAD. Family physicians, internists, physician assistants, nurse practitioners and vascular specialists can all diagnose PAD by examining a patient’s medical and family history, performing a physical exam, and conducting diagnostic tests. PAD can be diagnosed through a variety of diagnostic procedures including:
- Ankle-brachial index (ABI):A common test used to measures the difference between blood pressure at the arm and at the ankle. A difference in the two areas indicates restricted blood flow.
- Ultrasound
- CT and MR angiograms
- Angiography
- Blood tests
Treatment
Over the past 15 years the interventional treatment of peripheral arterial disease (PAD) has changed significantly. Endovascular techniques have replaced many traditional open surgically invasive procedures as the dominant intervention. More recently, pedal access techniques, accessing the blocked area from the toe versus a traditional access point in the patients groin, has shown, in certain instances, to be significantly more successful that earlier methods of revascularizing the impacted area. Dr. Kokinos has performed more pedal access approach procedures that anyone in Northern California and because of this she able to provide patients with more options for treating their disease than many other surgeons.There are multiple options for treatment of PAD, ranging from medical interventions, surgical revascularization, and endovascular therapy. Vascular Surgeons are uniquely qualified and trained to treat patients diagnosed with PAD. Approaches to treatment include:
- Minimally invasive endovascular procedures
- Medical management
- Exercise and lifestyle modifications
- Surgical bypass Amputation
Early detection and treatment are important to control the disease and to allow patients a full selection of treatment options. If you suffer from non-healing leg wounds and or have difficulty walking short distances, ask your physician if you can have a vascular ultrasound study to evaluate your risk of PAD.
South Bay Vascular Center and Vein Institute is the recognized as the regional treatment center for the treatment and care of patients suffering from Peripheral Arterial Disease. Dr.’s Kokinos’ specialized training and state of the art interventional facility offers patients a unique alternative to a hospital setting and provides the highest level of care for the treatment of PAD as an alternative to limb amputation.
If you or a loved ones suffers from PAD, call our office today at 408-376-3626 to schedule a visit.
We offer hope when others say there is none.
www.southbayvascular.com