Hemodialysis is a type of dialysis where the patient’s blood is filtered through a machine. For hemodialysis, a vascular surgeon creates an entrance into the blood vessels, a “vascular access,” so that blood can flow to the machine, be dialyzed by a special filter, and then return to the patient.
South Bay Vascular is the only Bay Area dialysis access center staffed by local, full-time vascular surgeons and registered vascular ultrasound technicians. We are dedicated to providing cutting-edge care to our community and ensuring that all patients are treated with dignity and respect. We can help!
Three Types of Hemodialysis Vascular Access
There are three different ways to ensure good blood flow through the access. Because every patient is different, it is important to talk with your vascular surgeon to come up with the best plan for you. At South Bay Vascular, we use ultrasound technology to map the veins and arteries in your arms and have a thorough consultation with each patient before deciding on which type of access is the right fit.
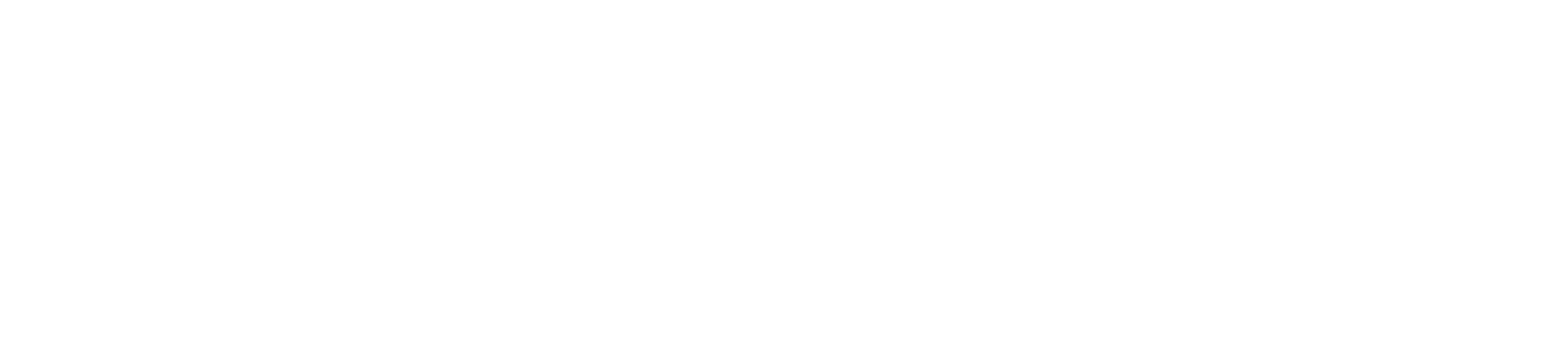
1Fistulas join your own artery and your own vein together, allowing the high-pressure flow from your artery to expand your vein and provide enough blood flow for dialysis. These are typically placed in the arm. A fistula is the preferred method of hemodialysis, according to the guidelines of the National Kidney Foundation; once it works, it tends to have the lowest complication rate and can be used for the longest time. However, it does take time for your vein to “grow and mature” into a fistula—usually about 4 months, though sometimes longer. Sometimes, especially in older patients, the vein simply doesn’t dilate properly. It is important to have close follow-up with your vascular surgeon once this fistula is created, both to ensure the best chance for it to develop, and to keep it working optimally.
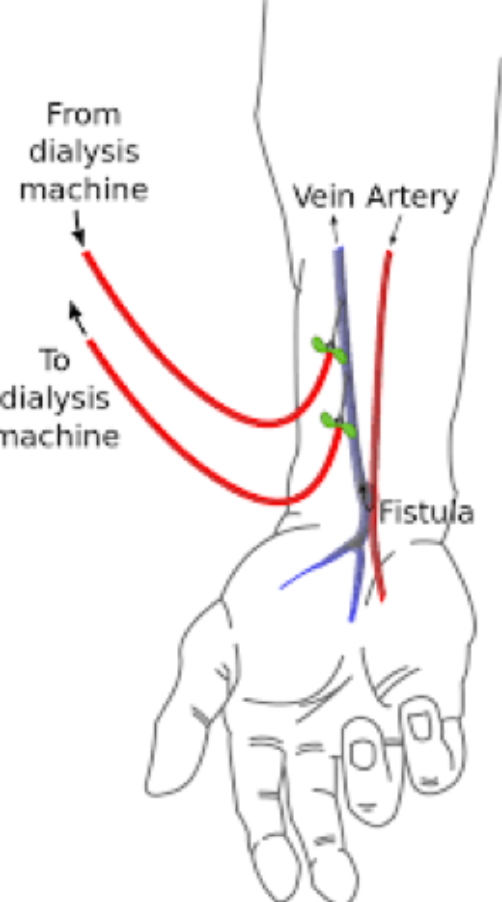
2Grafts use a manufactured tube to join your artery and vein together. These are usually made of Gortex (a plastic also used to make ski jackets) but can also be made from cow arteries or veins that have been specially sterilized. Grafts can usually be used about two weeks after placement. Complications include infection (which requires that the graft be removed) and thrombosis (blockage of the graft). Most grafts can be “declotted” or re-opened so that they can continue to be re-used.
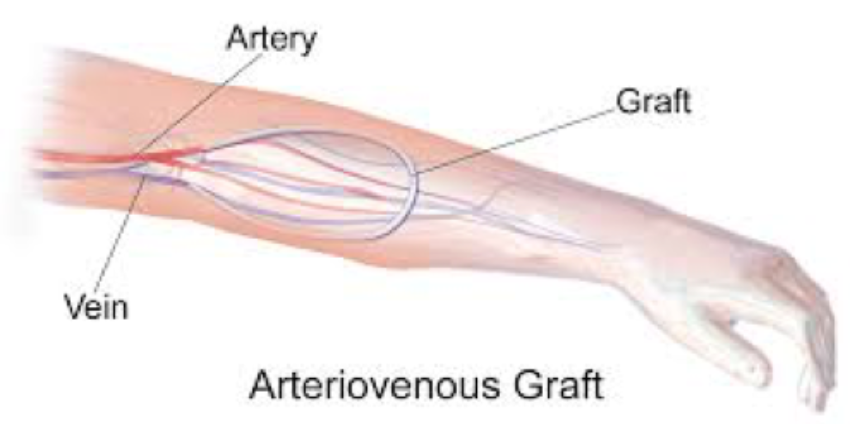
3Catheters are soft tubes placed in large veins, like large IV lines. Part of this tube is in the neck and part sits outside the body, usually on the upper chest. These are usually temporary devices used while waiting for an access to mature or heal or in cases where emergency dialysis is needed. There is a significant infection rate, so it is important to try to have a permanent access created as quickly as possible.
It is important to have good blood flow through the access. Every patient is different, so it is important to talk with your vascular surgeon to come up with the best plan for you. At South Bay Vascular, we use ultrasound technology to map the veins and arteries in your arms and have a thorough consultation with each patient before deciding on which type of access is the right fit.
Potential Complications
Patients often have hemodialysis sessions several times per week, meaning that their access is used regularly. Potential complications differ depending what type of access is in place but may include the following:
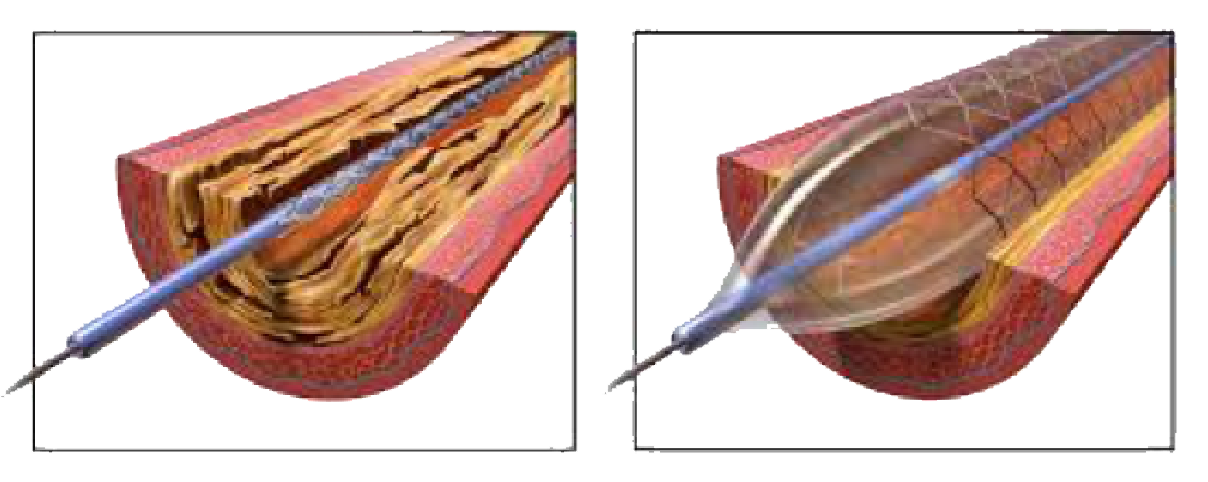
Stenosis or Thrombosis: With time and repeated use of any access, scarring of the access can occur. This can limit the amount of blood flowing through it, and this can decrease the ability to have good dialysis. Often, this can be evaluated with an easy and painless ultrasound and treated in an office or outpatient setting with a short procedure. This happens very commonly, and often repeatedly, in most dialysis patients.
Infection: Infection of the access is a feared complication, as it can make the patient extremely sick. It is most common with a catheter, as part of the plastic tube is inside and part is outside of the body. It is important to remove the catheter as soon as is possible and have a more permanent access created. With a catheter, infection can be sometimes treated with intravenous antibiotics (can be given on dialysis) and exchange of the catheter. If a graft becomes infected, it almost always has to be removed. Fistulas rarely become infected, because the access is the patient’s own vein.
Aneurysm Development: With fistula and some kind of grafts (those using cow vessels), the repeated trauma of needle puncture can weaken the wall of the fistula and cause it to dilate and make large “bumps.” These rarely cause a medical issue, but usually are just visually unpleasant.
Arm Swelling: If there is a narrowing in one of the veins in the upper arm or chest, the blood/fluid can back up into the arm and cause arm swelling. This problem can often be managed with a balloon dilation or stenting of that narrowed vein. Treatment is outpatient, but often needs to be repeated at intervals.
Hand ischemia: The fistula as it grows, or graft when it is placed, diverts some of the blood that would normally go to the hand to the access. In some patients, particularly those with diabetes, this can result in not enough blood going to the hand. This can cause fingers that are numb, cold, and painful, and may (rarely) develop gangrene. It is important to have this evaluated urgently by your surgeon if it happens.
Symptoms
It is important for patients to be aware of the signs to look for to protect their vascular access. If you notice any of the following, call your doctor or vascular surgeon:
- Alarms beep at dialysis
- Low blood flow rates
- Your hand feels numb or cold
- Prolonged bleeding after dialysis
- Swelling of your arm or hand
- Redness or warmth around your access
Regular Follow-Ups
Once an access is created, it is important to keep regular follow-ups with your vascular surgeon. At South Bay Vascular, we ultrasound your access on a regular basis to check the blood flow and look for any complications in order to keep your dialysis access healthy as long as possible. While some procedures must be done in the hospital for safety, we also have an on-site angio suite that allows us to do less-invasive, intravascular procedures in our clinic.
For more information about dialysis access issues, see our blog articles:


“I found Dr. Kokinos to be excellent at explaining, assessing, and treating. It is wonderful to find an excellent doctor who is also a friendly and compassionate person.”
– SBVC patient
“For over 12 months I went between UCSF and Stanford Clinics trying to get diagnosed because I was so ill...no one could ever find a cause to any of my symptoms....it turns out it was a blood flow problem that was making me so sick. I am very thankful I found Dr. Kokinos!”
– SBVC patient